Award or Grant: National Institutes of Health (NIH), R01EB002070
The Ballon lab has developed new methods for whole-body imaging of metastatic disease in oncology. The lab introduced a rapid, whole-body magnetic resonance imaging (MRI) technique for leukemia and metastatic cancers including prostate and breast cancer. The method is based, in part, on measurements of intracellular water self-diffusion coefficients. It requires no introduced contrast agents; can be performed in under 20 minutes; and is well suited to comparison with other whole-body assays like positron emission tomography (PET) and technetium (Tc)-99m bone scanning. Major applications include screening for disease, disease staging, therapeutic monitoring and understanding drug-delivery mechanisms. Unlike conventional bone scanning (tumor activity indirect measure), this technique is sensitive to the presence of intact disease vs. cells with cytotoxic therapy-compromised membranes.
The goals were to develop a non-invasive assay for characterizing hematopoietic activity in human bone marrow, and to test its utility monitoring and staging patients with hematologic malignancies. Presently, the needle aspirate and biopsy are used for definitive diagnosis and therapeutic monitoring. In addition to causing patient discomfort, biopsies and aspirates are limited to superficial areas of bone, such as the posterior iliac crest. This assay complements information obtained from the needle biopsy by providing a measure of the spatial extent of disease, particularly at sites inaccessible to the needle biopsy.
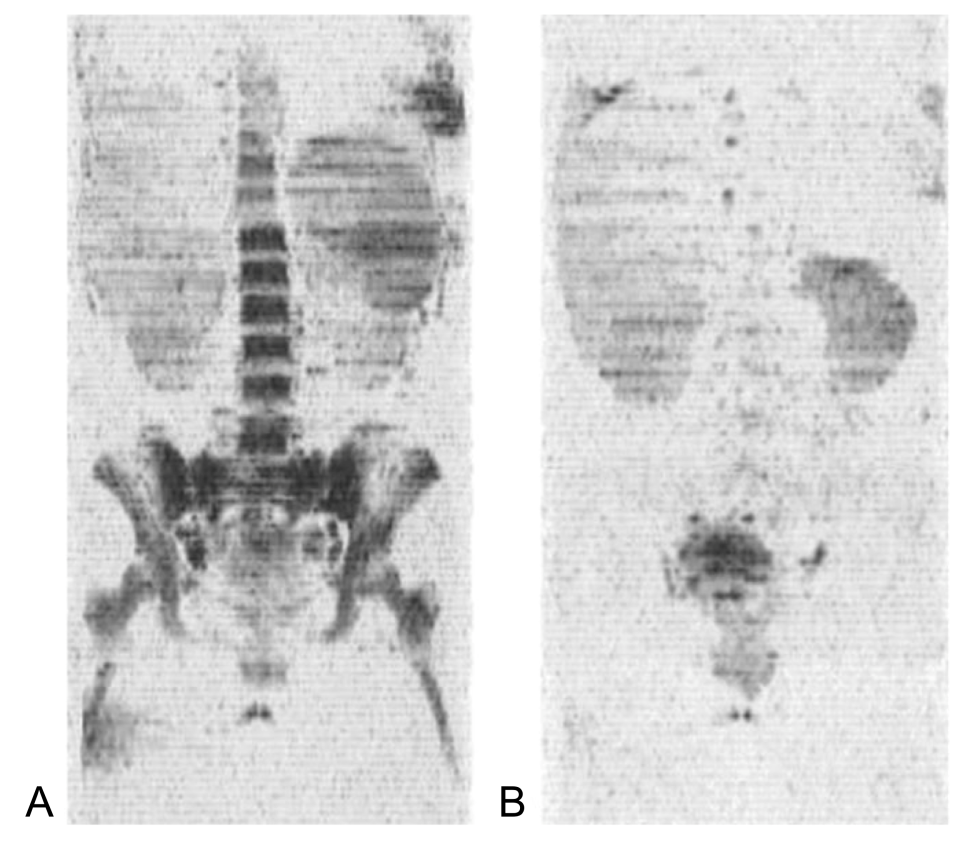
During this project, the Ballon lab demonstrated that nearly complete segmentation of leukemic bone marrow was possible using a high-speed MRI protocol with contrast based, in part, on the self-diffusion coefficient of intracellular vs. extracellular water. The segmentation quality was high enough to facilitate a projection-scan approach allowing a rapid assessment of disease extent. Earlier bone marrow studies by MR could not definitively detect leukemic infiltration, but measured changes related to bone marrow cellularity.
Full Caption: Acute myelogenous leukemia. (A) Coronal image from baseline study just prior to myelosuppressive therapy start. (B) Post-remission exam, 20 days later. The bone marrow was intact at baseline with a water fraction of 99% and a T2 of water equal to 62 msec consistent with leukemia. Twenty days post chemo initiation, the water signal in the bone marrow on T2- and diffusion-weighted images is virtually absent, marking a complete remission with only 2% myeloblasts on differential blood count.