Heart disease is the top U.S. cause of mortality, with 600,000 deaths annually. Its high prevalence is responsible for 1/6 of health care costs, which in 2010 were some $444 billion. Implantation of cardiac devices (pacemakers, heart valves, grafts, pumps) is the primary method of treatment for many cardiac diseases (coronary heart disease, atrial fibrillation, heart failure) due to the mechanical nature of the heart’s function. But many are ineligible for cardiac devices due to their ineligibility for open-heart surgery. Minimally invasive procedures based on cardiac devices deployed via catheters (i.e., transcatheter cardiac devices) avoid the need for surgery and decrease recovery time. Many fundamental transcatheter cardiac device limitations prevent their ubiquitous use in patients with structural heart disease: (i) a fixed geometry that can’t accommodate irregular heart anatomy, (ii) limited size number, and (iii) rigid materials causing stresses that damage tissue and prevent conformability. To overcome these limitations, a paradigm shift is needed in transcatheter cardiac device design principles and fabrication methods. This shift must focus on anatomy and clinically relevant imaging modalities.
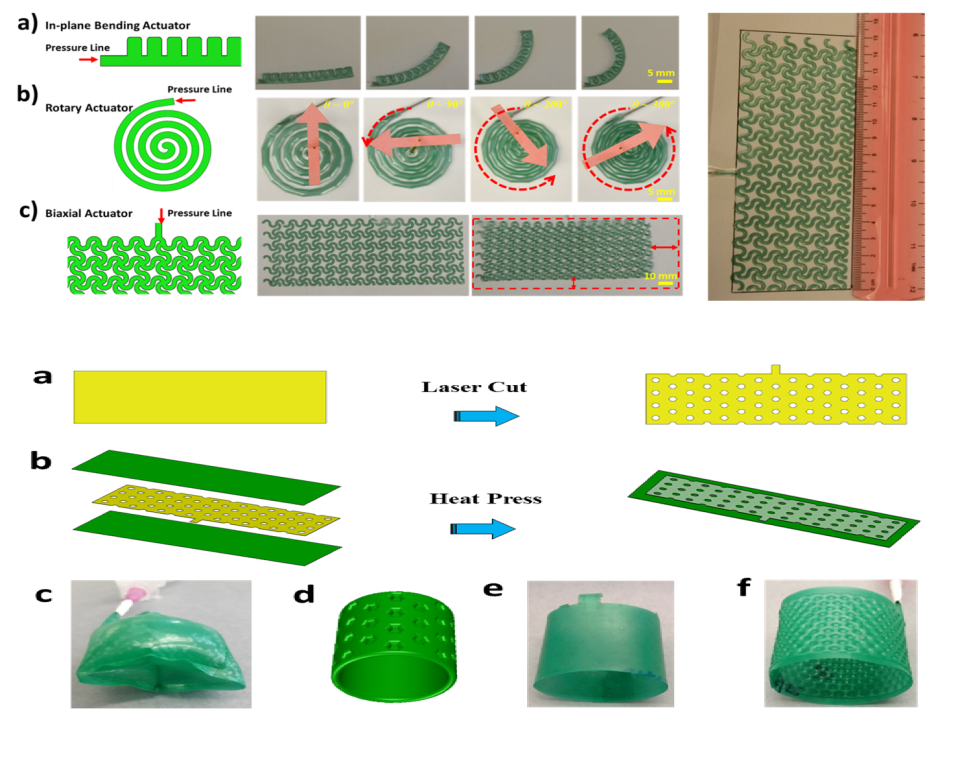
This project’s goal is to leverage sophisticated capabilities offered by soft robotics to develop transcatheter cardiac devices that accommodate the high variability of patient anatomy. Soft robotics uses elastomers that can undergo extreme volume changes (100-1000’s of percent) to build actuators capable of complex motions with simple inputs, due to the non-linear properties of the materials. Until now, most examples of this have involved creation of robots performing locomotion or gripping actions for applications in search and rescue missions, surveillance and payload delivery. But soft robotics is well suited for medical applications as the inherent compliance of the actuators matches that of soft tissues, providing safe interfaces. The technology offers a simple method for conforming devices to variable anatomy. Soft robotic devices can also be fabricated from rapid prototyping (e.g., 3D printing, laser cutting), allowing for structures of arbitrary geometry, based on 3D designs generated from medical images. Made in an inflatable form factor, they can easily be made to fit within catheters in their deflated state, then inflated with a thermal curable liquid permanently holding a geometry conforming to anatomy.
The lab demonstrates the application of soft robotics to several device classes, including stents, valves and pumps. The devices prove functional on benchtop models. The work is the foundation for the project developing a soft robotic mapping catheter for atrial fibrillation.