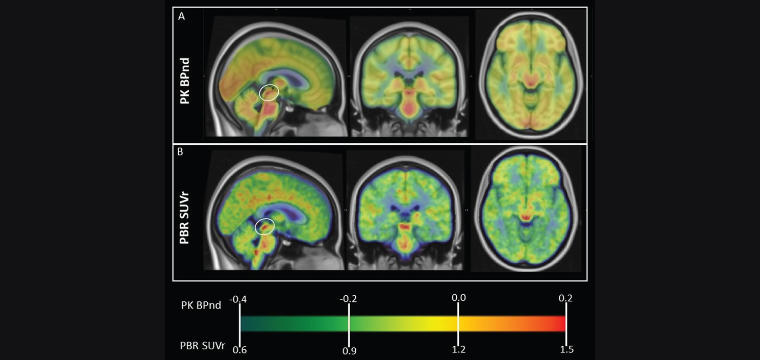
Alzheimer’s disease (AD) pathology is thought to begin in the brainstem — the brain’s evolutionarily oldest part, which is vital for basic life functions, and, in humans, where tau first accumulates, slowly initiating the AD process. Cerebral microglia, the central nervous system’s most prominent immune cells — the first to respond when the brain goes awry — play a critical role in AD pathogenesis, yet little is known about brainstem microglia in AD. Translocator protein positron emission tomography (TSPO PET), which is sensitive to activated microglia, shows a high signal in the dorsal human brainstem; still, the signal’s precise location and clinical correlates are unknown. So, a Brain Health Imaging Institute (BHII) team sought to define age and AD association of brainstem TSPO PET signal in humans. Their research, “Reduction in Constitutively Activated Auditory Brainstem Microglia in Aging and Alzheimer’s Disease,” was recently published in the Journal of Alzheimer’s Disease.
“The study uncovered a surprising and unusual pattern of neuroinflammation in the brainstem of living humans,” said Tracy Butler, M.D., Associate Professor of Neurology in Radiology and the paper’s first author.
Neuroinflammation, measured using TSPO PET, is usually considered harmful — a sign of disease. Typically, AD and aging are linked to abnormally high microglial activation in most cortical and subcortical brain regions. But that’s not what BHII found.
“Our study found the opposite pattern in the brainstem,” said Dr. Butler. “AD was associated with markedly reduced microglial activation, especially in the inferior colliculi, a region critical for normal hearing. Neuroinflammation in this region also declined significantly with aging. This indicates that microglia may play a completely different role in the brainstem than the rest of the brain. Activated microglia appear to be beneficial and possibly essential in the brainstem.”
The results suggest a unique role for brainstem microglia, particularly in the midbrain, where nuclei involved in early sensory processing are adjacent to nuclei where AD pathology begins. Further studies using higher-resolution techniques, including animal models and postmortem human brain tissue, are needed to better understand this role.
“We hope our intriguing and unexpected PET results call attention to the importance of brainstem microglia, which have received limited scientific attention to date,” says Dr. Butler. “A better understanding of brainstem microglia could explain strong links between sensory loss and AD. It could improve AD diagnosis, treatment, and maybe even prevention.”

